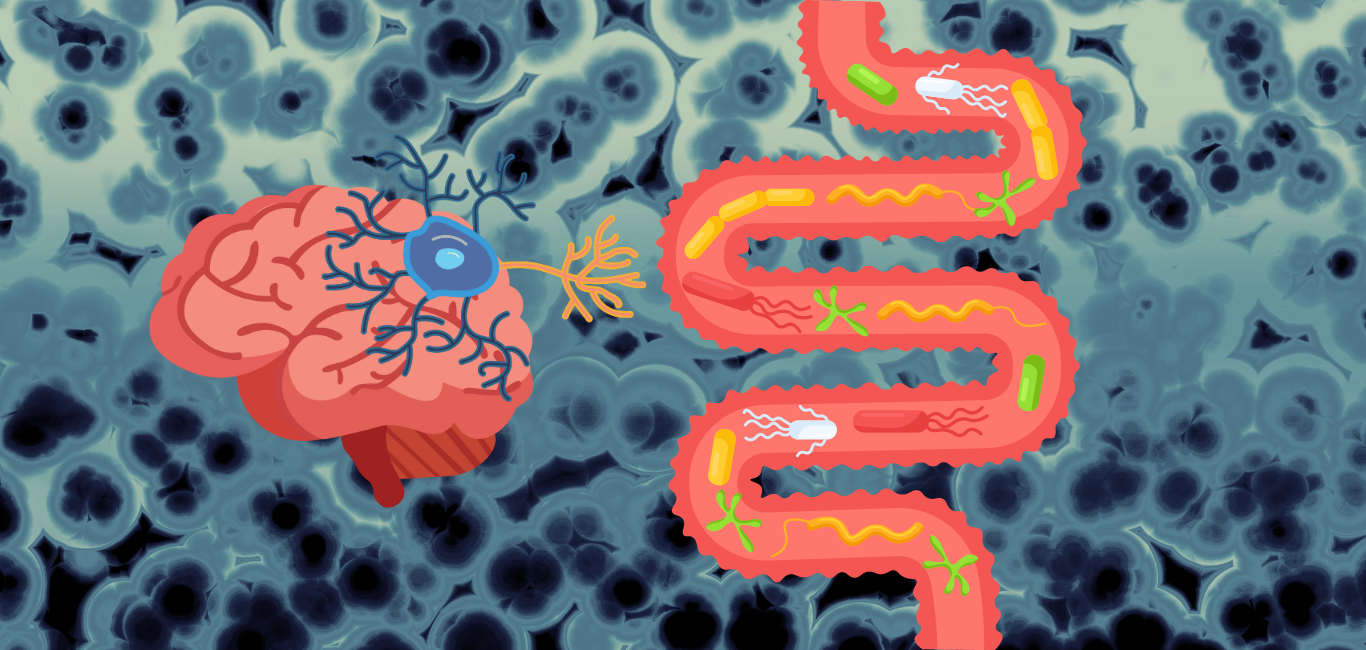
Efforts to unravel the gut-brain relationship have broadened the horizons for understanding and finding potential treatment options for several neurological conditions. A new study from the Washington University School of Medicine, USA, has sought to examine this relationship further on how the gut microbiome affects the degenerative process in Alzheimer’s disease.
In their experiments on mice, the researchers noticed significant changes in the characteristics of Alzheimer’s disease when they altered the bacteria in the guts of the mice.
“When we either remove the bacteria that live in the intestines or modify them, it can strongly protect brain damage like that seen in Alzheimer’s disease,” David M Holtzman, professor of neurology at the Washington University School of Medicine and the study’s corresponding author, tells Happiest Health.
In Alzheimer’s disease, there is sequential build-up of two types of toxic proteins in the brain: amyloid beta followed by complex tau threads. A build-up of the tau protein causes the neuron to shrink and eventually die, manifesting as cognitive decline.
Gut, brain and the APOE4
Studies have found an interplay between the gut microbiome and a key Alzheimer-risk gene called APOE4. APOE genes carry the information that makes a protein called apolipoprotein E which in the brain is responsible for maintaining the health of the neurons. APOE4 specifically drives the tau to pile up by influencing inflammation in the brain.
Read more: Decoding the genetics of Alzheimer’s: the role of APOE4 and SHMOOSE
These studies have shown that certain types of bacteria in the gut can alter APOE4 levels. However, how the gut microbiome drives tau accumulation remains a mystery, which is what the current study scientists wanted to solve.
Untampered by tau
The scientists divided the mice into two groups: one grew in a normal environment and the other in a sterile germ-free environment. Then, they modified the APOE4 genes of both groups of mice so that their brains were susceptible to tau aggregation.
In the mice which were kept in the normal environment, they noticed their brain had more tau protein.
Next, they treated the mice in the regular environment with antibiotics for one week. The mice were protected from degeneration caused by the tau protein. This is because the antibiotics reshaped the bacterial community in their gut in a favourable way.
However, they did not study the consequences of long-term antibiotic use and gut microbiome in relation to Alzheimer’s.
The scientists also observed that certain bacteria in the gut, such as Ruminococcaceae and Lachnospiraceae, produced specific molecules called short-chain fatty acids (SCFA), which exacerbated tau accumulation.
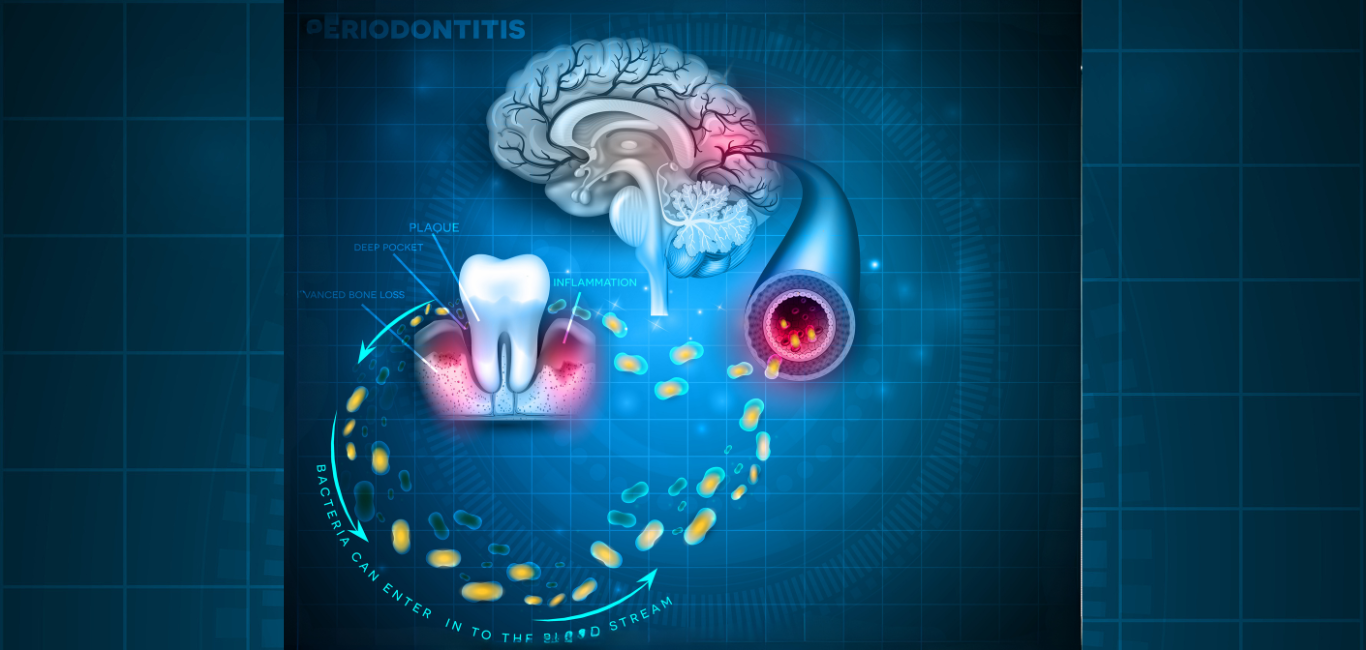
The researchers’ hypothesis is that these SCFA molecules trigger the body’s immune system. This in turn activates the brain’s immune cells causing inflammation. The inflamed condition prompts the tau proteins to accumulate.
Read more: Secret allies: the brain and the immune system
The antibiotics also reduced the number of glial cells – which are the brain’s immune cells. They also lessened the production of short-chain fatty acids, which proved to protect the mice.
In contrast, the mice in the sterile environment did not develop the tau threads.
Worth probing further
David Vauzour, associate professor of molecular nutrition at the University of East Anglia, UK, says, “The current study suggests that the gut microbiome is worth investigating further. It is a potential target to mitigate the deleterious impact of the APOE gene in preventing Alzheimer’s disease.”
Dr Vauzour’s lab works on developing novel dietary and therapeutic strategies to delay brain ageing, cognitive decline and neurodegeneration.
The concept of altering the gut microbiome for treating neurodegenerative disorders is still in its infancy. Nevertheless, Prof Holtzman still holds hopes. “Our study suggests that treatments that influence the microbiota, such as certain probiotics or bacteria might be something to consider. Further studies are needed to test whether this might have beneficial effects,” he adds.
Dr Vauzour agrees. “Manipulating the gut microbiome is an attractive therapeutic strategy to consider mitigating neurodegenerative disorders. Future studies are warranted to assess this strategy further,” he says.