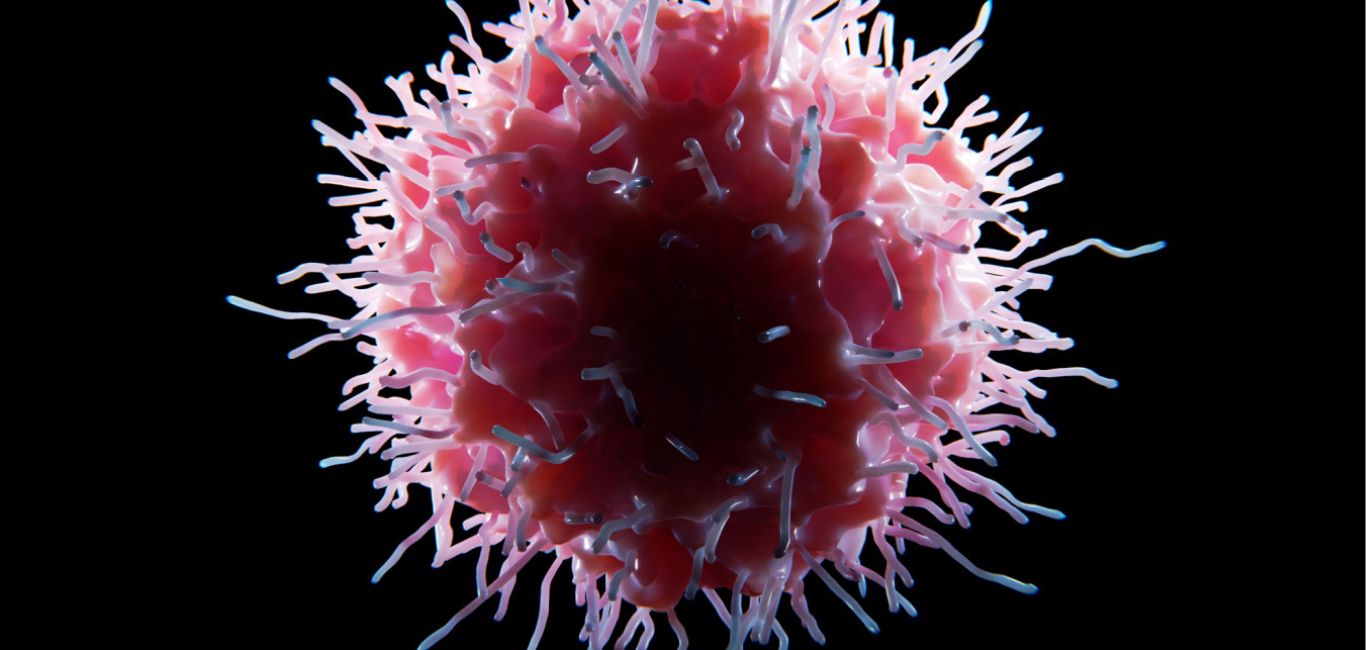
You have probably heard of T-cells, a vital component of our immune system. But there is another special kind called the ‘gamma delta’ (γδ) T cells that have a unique power to help fight cancer.
Gamma delta T cells recognize cancer cells and instruct other immune cells to join the battle against cancer.
Researchers have now figured out how to use the tiny particles that gamma delta T cells release, called extracellular vesicles (EVs), to make cancer vaccines.
EVs have been used in vaccine research for a while, especially against bacterial infections, since the 1980s. Professor Kenneth Witwer from the Johns Hopkins University School of Medicine has been studying how to use EVs in vaccines. His lab recently published research on an EV-based vaccine derived from Salmonella bacteria, which proved to be both effective and stable in fighting SARS-CoV-2, the virus that causes COVID-19. This shows the potential of using EVs in developing vaccines.
Smart missiles seek cancer cells
Comparing extracellular vesicle-based vaccines to traditional vaccines is like contrasting smart missiles with unguided bombs. Traditional vaccines work broadly, while extracellular vesicles (EVs) precisely target cancer cells, minimising the risk of collateral damage. EVs can effectively transport specific tumour antigens (TAAs) and enhance targeted T-cell responses against cancer.
EVs derived from immune cells exhibit high compatibility and contain crucial molecules for presenting antigens to T cells without relying on antigen-presenting cells. This results in faster immune responses. Additionally, the exosome membrane features `do not eat me’ signals, contributing to their immune evasion properties.
“Taken together, extracellular vesicle-loaded antigens offer a significant advantage over traditional antigen vaccines,” says Dr Jyotirmoy Rakshit from the University of Texas Health at Houston, highlighting the potential of this approach in the field of vaccination and cancer treatment.
“The EV itself is what sets it apart. It serves as a ‘signalling platform’ that presents the antigen in a specific molecular context,” explains Professor Witwer.
Think of EVs as delivery vehicles of our body’s immune system. They transport essential information and enhance our body’s response to threats. Some components of EVs facilitate good interactions between cells and antigens, and they can also carry substances that either amplify or dampen the immune system’s activity — a role that the antigen cannot fulfil on its own.
A study unveils promising results
In a recent study published in the Journal of Extracellular Vesicles, scientists used gamma delta T cells to create a powerful weapon against the Epstein-Barr virus* EBV, which can lead to cancer. They collected gamma delta cells and dendritic cells from a human donor. The gamma delta cells released EVs loaded with EBV tumour antigens.When presented to dendritic cells, it triggered them, acting like a vaccine.
These EVs, filled with tumour-fighting tools, are now a gamma delta γδ-T-EVs-based vaccine. When they tested this vaccine on mice with EBV-related tumours, it worked well, killing tumour cells and improving the immune system response.
The future of EV-based vaccines
This implies that the extracellular vesicles from gamma delta T cells are considered part of the body (‘self’), which is why they do not trigger a strong immune response.
This means the extracellular vesicles from gamma delta T cells are considered part of the body (‘self’), which is why they do not provoke a strong immune response. This quality suggests a low risk of side effects, making them safe for potential medical use.
In the future, it may become necessary, similar to blood transfusions, to select extracellular vesicles that are compatible with individual recipients, says Prof. Witwer.
Personalised therapy
Matching extracellular vesicles to individual recipients is similar to the idea of personalised medicine, where treatments are customised for each person’s unique characteristics and needs.
Dr Rakshit is also hopeful of this scenario and says, “Personalised cancer immunotherapy, involving surface antigen engineering and tailored therapeutic antigens, remains a promising avenue but necessitates further research and clinical validation.”