Gastrointestinal issues encompass a range of disorders, with two prominent ones being irritable bowel syndrome (IBS) and inflammatory bowel disease (IBD). Although they both affect the intestines, it is crucial to recognise the distinct nature of these conditions in terms of their presentation, diagnosis and treatment.
“While they both affect the intestine, there is a lot of difference in the symptoms as well as the trajectory that both diseases take,” says Dr Vineet Ahuja, a gastroenterologist at the All-India Institute of Medical Sciences (AIIMS), Delhi.
IBS is a “motility or a stress-induced disorder”, says Dr Ahuja, adding that it is characterised by symptoms that tend to follow a cyclical pattern. These symptoms can persist for a certain period and can recur after a period of remission.
IBD is a more severe condition than IBS and entails inflammation and structural damage to the gastrointestinal tract. It encompasses two primary conditions: Crohn’s disease and ulcerative colitis.
Causes

The exact cause of IBS is not known although studies point to a combination of factors that include hypersensitivity, stress, bacterial infections, changes in the gut microbiome and food sensitivities. IBS is heavily influenced by how the gut and the brain talk to each other. It can be aggravated by stress.
IBD has a genetic and environmental component to it. Its symptoms arise from an abnormal immune response in the gut which damages the tissue. “It’s a kind of autoimmune [disorder] where the body starts reacting against its own gut bacteria. [It] perceives it as threat leading to inflammation and causes ulcers,” says Dr Ahuja.
Symptoms
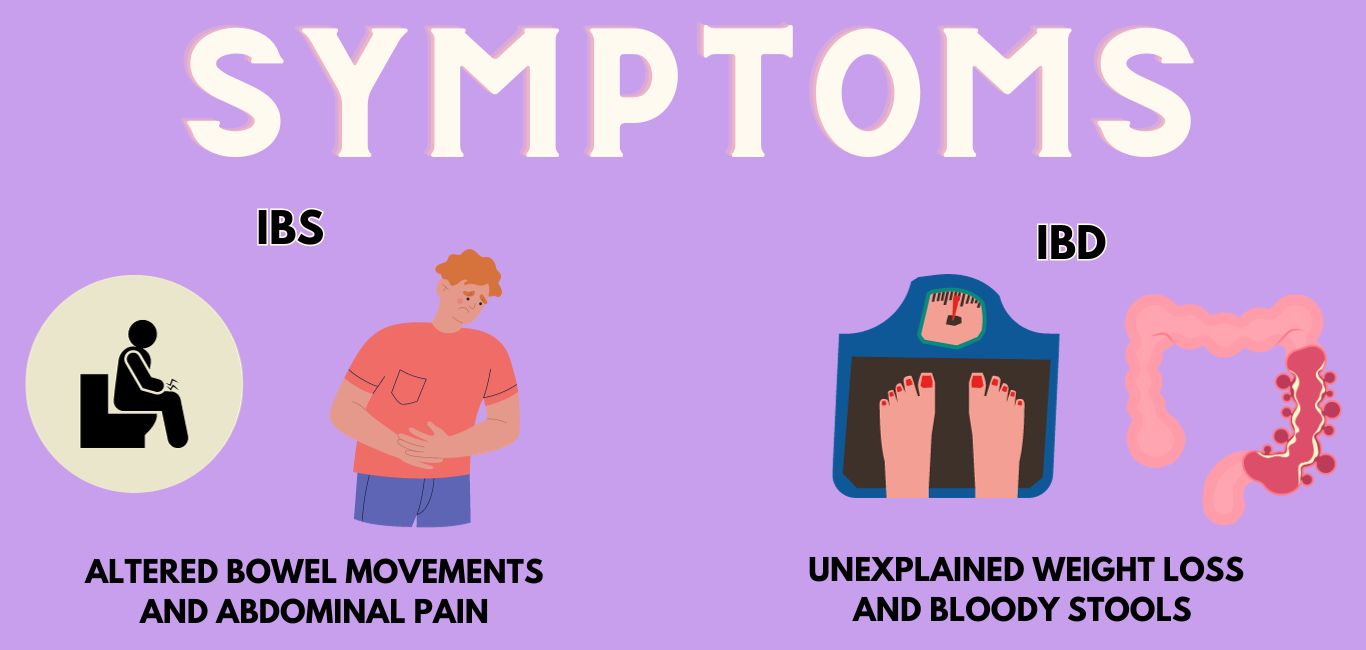
The symptoms of IBS can include:
- abdominal pain that goes away after defecation
- altered bowel movements
- fluctuating symptoms of diarrhoea and constipation
- bloating
- flatulence or excessive gas
IBD symptoms include:
- loss of appetite
- weight loss
- fatigue
- fever
- bloody stools
- anaemia
Diagnosis

Both IBS and IBD can be diagnosed with the help of blood tests and a visual examination of the colon through a colonoscopy. However, in the case of IBS, any blood tests will show normal parameters, says Dr Ahuja.
“For IBD, the blood testing parameters for haemoglobin, serum albumin and serum proteins will be low with a high ESR and C-reactive protein level,” he adds. Further, a colonoscopy shows a normal intestine in IBS cases; whereas in IBD, ulcers and other features of inflammation will be seen.
Treatment and management
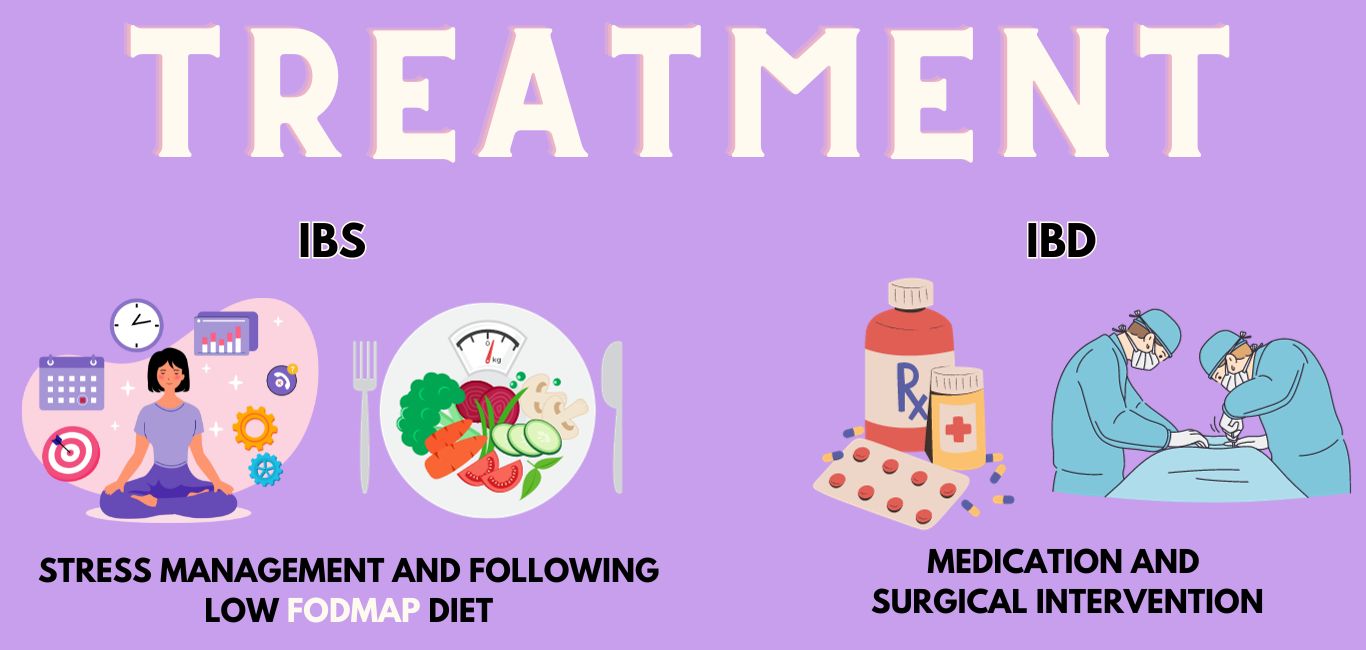
“IBS requires intermittent symptomatic therapy where medication is given as and when [symptoms] show up,” says Dr Ahuja. It can be managed with dietary interventions such as a low consumption of FODMAP, besides managing stress and anxiety levels.
(FODMAP is an acronym for a set of short-chain carbohydrates – fermentable oligosaccharides, disaccharides, monosaccharides and polyols – which may not be absorbed well by the small intestine.)
“IBD requires lifelong treatment with immunosuppressive medication along with drugs like monoclonal antibodies” says Dr Ahuja. to manage complications of the condition. Complications include development of fistula (abnormal connections between organs or tissues) and abscess.
IBD may warrant enteral nutrition, or tube feeding, to deliver nutrients to the stomach. This is because protein absorption is low, says Dr Ahuja.