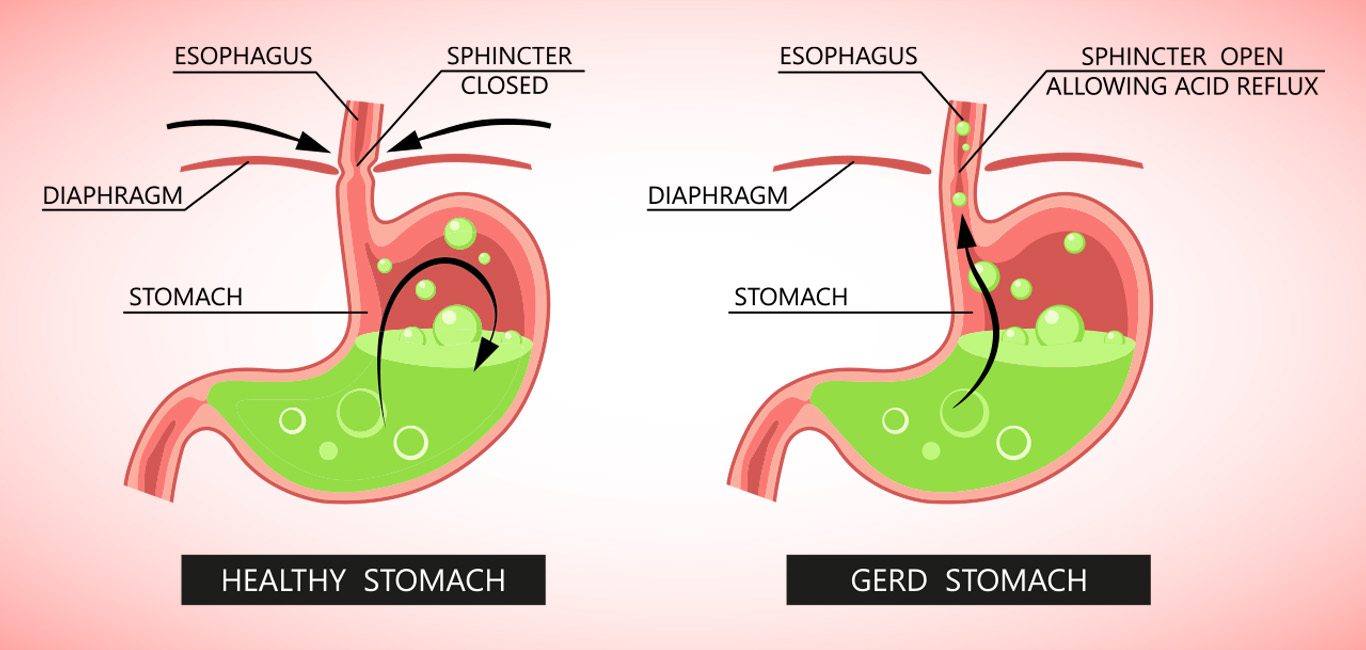
Gastro-esophageal reflux disease (GERD) occurs when the acidic content of the stomach gets flushed frequently into the oesophagus, the tube that connects the mouth and stomach. It is a chronic symptom of damage to the lining of the oesophagus due to the reflux of acidic content (acid reflux) from the stomach.
This acid reflux happens due to a defect in the ring-shaped lower esophageal sphincter (LES) muscle present at the junction of the oesophagus and stomach that regulates the opening and closing of a valve.
Signs and symptoms
The most common identifiers of GERD are:
- Heartburn is caused by the acid reflux that irritates and damages the oesophageal lining, causing a burning sensation. This usually happens after eating or lying down. Sometimes, it can cause chest pain that could be confused with a heart attack
- Regurgitation caused by acid reflux that usually causes a sour and unpleasant taste in the mouth or throat
- Dysphagia or difficulty in swallowing
Persons suffering with GERD can also experience:
- Hiccups that keep coming back
- Feeling of lumps in the throat
- A hoarse voice
- Bad breath
- Bloating
Causes
GERD happens due to a defect in the LES muscle causing acid reflux. The LES muscle either relaxes abnormally or weakens, allowing the backflow of stomach acids into the oesophagus. There are certain other factors that can increase the risk or aggravate GERD. These include:
- Obesity
- Excessive consumption of caffeine through coffee, chocolates
- Excessive smoking and alcohol intake
- Pregnancy
- Intake of fatty and oily foods
- Hiatal hernia (bulging of the upper part of the stomach into the diaphragm)
- Certain medications like paracetamol, aspirin, ibuprofen, etc.
Diagnosis
GERD can be diagnosed by reviewing a person’s history of symptoms along with evidence from certain procedures that include:
- Endoscopy – used to check whether the lining of the oesophagus is damaged or not
- Barium swallow – used to assess a person’s ability to swallow and find the location of the problem
- Manometry – used to assess how well the LES is working
- Esophageal pH monitoring – can assess the acid and non-acid reflux by using a catheter or inserting a wireless capsule in the oesophagus
Treatment
Lifestyle modifications are essential to treating GERD. These include:
- Limiting caffeine intake
- Stopping to smoke and consume alcohol
- Switching to a fibrous diet and eating less in a single sitting
- Losing weight
Treating medical conditions like hiatal hernia can also help to get rid of frequent acid reflux and better manage GERD. In case where lifestyle modifications are not improving the symptoms, a doctor can prescribe oral medications of different classes as standalone or in combination. These include:
- Antacids, which neutralize the acid in the stomach such as aluminium hydroxide, magnesium carbonate, sodium bicarbonate
- Proton pump inhibitors (PPIs), which block the secretion of acid in the stomach such as pantoprazole, rabeprazole, etc.
- H2 receptor blockers, which block the secretion of acid in the stomach but are less potent than PPIs, such as ranitidine, cimetidine, etc.
Sources