The delicate nature of the brain is a reason why any disturbance to it can cause cognitive impairment or other side effects.
It has been established that an invading brain tumour compromises brain function and decreases the quality of life of the individual. A medically accepted assumption is that the mass of the tumour causes this neurological dysfunction.
Spanish cancer researcher Dr Manuel Valiente discovered something different as he pursued a lingering thought as to how a large tumour sometimes caused a relatively smaller effect than a smaller tumour.
“Referring to this neurocognitive impact, [doctors] were unable to explain why a person with a huge metastasis does not have any symptoms while another patient with a tiny met (tumour) is unable to move,” says the lead researcher from the National Cancer Research Center or CNIO, Madrid. (Metastasis is an advanced stage of cancer which has spread beyond the organ which it first affected.)
His team found that brain tumours chew into the chemical and electrical activities of the surrounding neurons and affect their communication and function.
Changes in brain communication
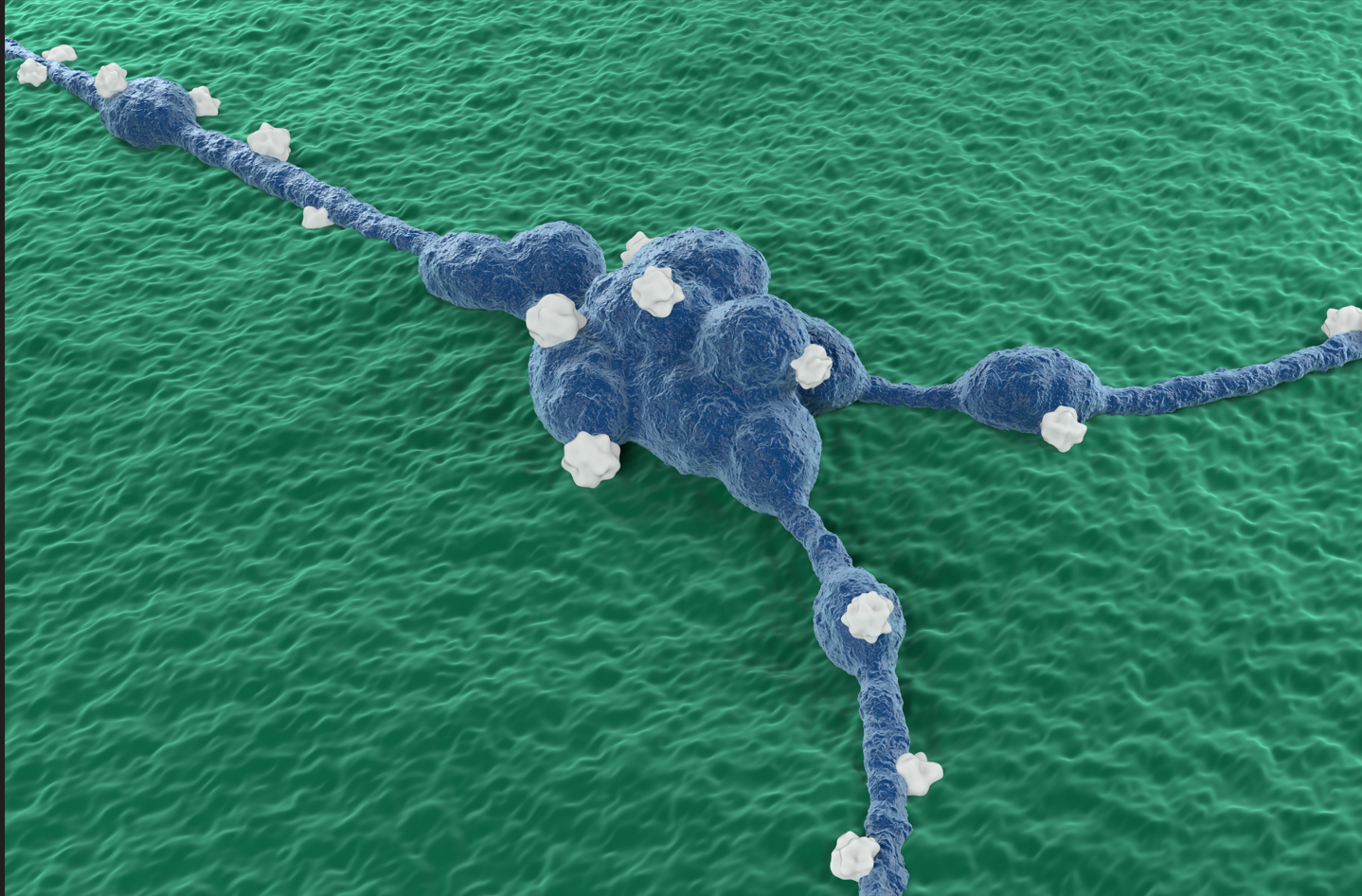
Dr Valiente and another Spanish researcher, Dr Liset M de la Prida from the Instituto Cajal, Spain, used an integrated molecular and electrophysiological approach to explore this debilitating molecular cross-talk between the tumour and neurons. They observed chemical and electrical changes in the neurons surrounding the growing brain tumour.
This find challenges the ‘mass effect’ theory, which says the size of the tumour alone causes neurological dysfunction.
“The mass effect was completely incompatible with what we were seeing [under] the electron microscope,” says Dr Valiente. Instead, the researchers noticed that the type of tumour disturbed the electrical communication between neurons.
Dr de la Prida’s team members used probes to measure the electrical activity in mice with and without brain metastasis and observed a difference.
They trained an algorithm with multiple electrophysiological recordings and then ran their readings. It confirmed their observations that tumours did, in fact, affect the brain’s electrical activity in a recognisable pattern.
“Machine learning provides different predictive models,” says Dr de la Prida. She explains that the machine learning models were trained on electrophysiology readings to classify types of tumours. This can, in turn, predict the stage and type of tumours based on new electrophysiology readings.
Brain tumours cause molecular changes
To study the molecular changes that alter the neural electrical activity, the researchers did a genetic analysis of tumour samples from humans and mice. From this exercise popped up a candidate molecule – the EGR1 — as a potential protein causing the changes.
EGR1 or early growth response protein is essential in synaptic plasticity and neuronal communication. “[It is] interesting because [EGR1] is known to be involved in the regulation of synaptic activity, and also it’s known to be involved in processes of vascularisation and regenesis,” says Dr Valiente. In other words, EGR1 also plays a key role in the blood supply to and growth of neurons in the brain.
Read more: Astrocyte’s new-found cells may be game-changers in neuroscience: Study
By changing electrical and molecular activities, the tumour also alters functioning in neighbouring brain regions, thus affecting cognition.
New ways of diagnosis
Can affected persons regain their cognitive functions once the tumour is removed? Dr Valiente seems sceptical. He explains that although the brain is `plastic’, i.e. capable of reorganising and adapting its neurons, it cannot repair itself as other organs can. Nevertheless, he asserts, their finding opens new diagnostic avenues for brain tumours.
To understand how different subtypes of tumours change brain function, Dr Valiente and his team are testing fresh tissue samples and collecting data in collaboration called RENACER with 18 hospitals in the UK. He expects that the electrophysiological readings, at some point, would help diagnose the presence of a brain tumour and its subtype.
In his view, “[It] might one day become a model that we can also intervene with electrophysiology for patients. If we can go early enough, we can maybe predict what will happen with that metastasis. Or [how] this metastasis will behave in terms of the neurocognition.”
The researchers have also created a novel platform that can give a better drug screening against tumours than current ones.
They aim to follow up their study on EGR1 from the therapeutic perspective and find more such proteins for potential drug targets.