They could be enzymes that ensure specific reactions happen smoothly or they could be hydrochloric acid in the stomach that break down the components of food. No matter their form, chemicals in balanced amounts are paramount in the proper functioning of the human body. In the brain, the chemical paraphernalia are neurotransmitters. These ensure adequate communication between the nerve cells and govern various aspects like mood, emotions, body temperature, heartrate, even digestion.
Read more: The fascinating symphony of neurotransmitters
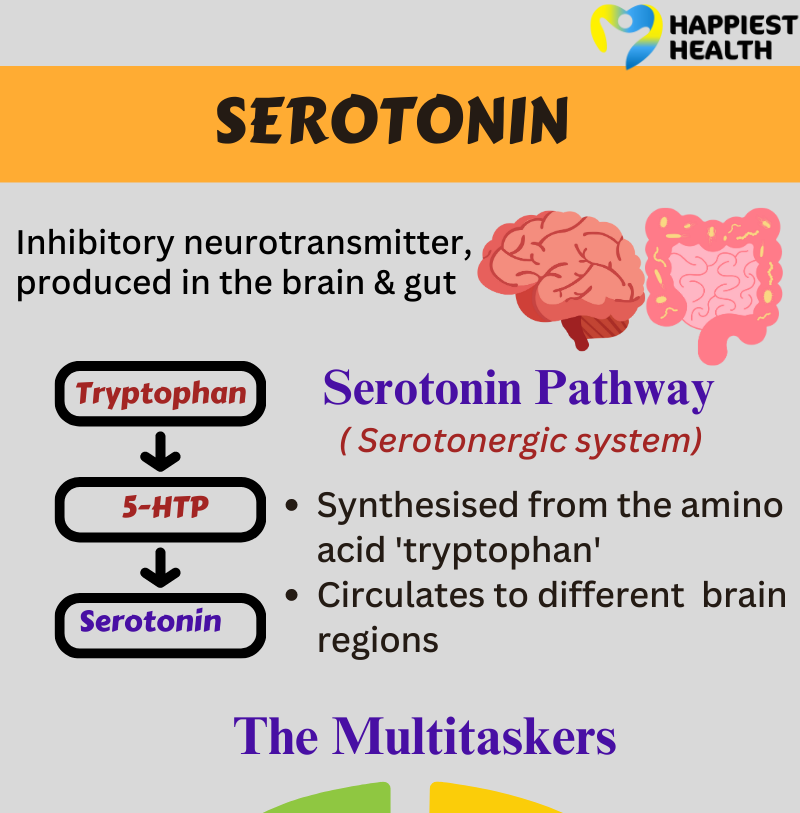
One such neurotransmitter is serotonin, which gets the moniker of ‘the happy hormone.’ The body’s natural feel-good chemical governs feelings of happiness, satisfaction and optimism. “Multiple human behaviours and moods are regulated by serotonin,” Dr Sneha V, a consultant neuropsychiatrist based in Bengaluru, tells Happiest Health.
Beyond the happy hormone
Serotonin is a multifaceted neurotransmitter that plays a role within and outside the central nervous system. This neurochemical is derived from the amino acid tryptophan. It is produced by specialised cells in the gastrointestinal tract and the raphe nuclei of the brainstem. “In our brain, serotonin helps regulate attention and moods in depression and anxiety. It is also involved in appetite, nausea, regulating temperature and muscle tone,” says Dr Sneha.
Read more: Serotonin: the key to happiness and well-being
Serotonin maintains the structure of blood vessels and uterine muscles outside the central nervous system. It helps the movement of food in the gastrointestinal tract. It also aids in clotting of blood, as it is found in platelets.
Dr Sneha further explains that when serotonin levels dip, it could lead to aggression, clinical depression and anxiety. Increasing serotonin levels becomes the motive of many antidepressant medications like selective serotonin reuptake inhibitors (SSRIs) and monoamine oxidase (MAO) inhibitors. SSRIs prevent serotonin reuptake in the cell, ensuring it remains between the synapses. MAO inhibitors prevent the breakdown of serotonin in the liver. Hence, these medications can help manage symptoms of depression and anxiety.
A loss of balance
There is a flip side to serotonin, too. Just as too much of a good thing can turn detrimental, serotonin concentrations between the synapses increase when the brain’s happy switch, or the activity of serotonin, remains on for too long. This results in a potentially life-threatening phenomenon, serotonin syndrome, often a drug-induced condition.
And intentional or unintentional overuse of medications like SSRIs, opioid painkillers and MAO inhibitors exacerbate the condition. “If the individual is using a drug that inhibits the enzyme that metabolises serotonin, such as the class of MAO inhibitor antidepressants, then there’s a possibility of the syndrome occurring,” says Dr Silvana Chiavegatto, assistant professor at the Department of Pharmacology at the University of São Paulo, Brazil.
Dr Sneha enlists some common symptoms seen in serotonin syndrome:
- restlessness
- disorientation
- agitation,
- anxiety
- some muscular abnormalities like tremors and rigidity
- increased blood pressure (hypertension)
- higher heart rate (tachycardia)
- nausea
- flushed skin
- increased bowel sounds
“Increased serotonin signalling can induce symptoms of the syndrome and interfere with the signalling of other neurotransmitters, such as norepinephrine,” Prof Chiavegatto adds. This could account for peripheral symptoms like hypertension and tachycardia.
Close and accurate diagnosis
Studies find that many symptoms of serotonin syndrome correlate with other disorders like alcohol withdrawal and neuroleptic malignant syndrome. Prof Chiavegatto explains that three defined diagnostic criteria — Sternbach, Radosmki, and Hunter — help determine if the person has serotonin syndrome. Experts usually assess the person’s altered mental health status, hyperactivity and neuromuscular abnormalities. They also look at the type, combination and dose of the serotonin-boosting medication the person has been taking.
However, this syndrome is not usually seen in everyone who takes these serotonin agents. “We comprehend its manifestation, but we are yet to grasp why certain individuals develop the syndrome, while others on identical medication don’t,” says Prof Chiavegattto. She proposes that the discrepancy could be due to different gene structures of the enzymes breaking down the medication. This difference could elevate blood concentrations of the serotonin-boosting agent beyond therapeutic levels.
Tackling the syndrome
When serotonin syndrome is caught early, treatment is quite simple: just removing the causative medication/s is sufficient, says Prof Chiavegatto.
She recounts an incident where one of her PhD students met a person in their late 60s who had been taking SSRIs for several years. He was at the hospital due to a urinary tract infection. He had to be moved to the ICU (Intensive Care Unit) as he was experiencing mental disorientation, excessive sweating, and hypertension. The student took the person off the SSRIs, and all his symptoms went away in 24 hours; after a few days, the person was discharged.
However, managing the condition varies based on its severity. In moderate cases, experts find ways to manage the respiratory and cardiovascular symptoms and discontinue the medication. If there are more severe neurological and physical symptoms, it calls for more intensive care and attention.
Takeaways:
- Serotonin syndrome is a drug-induced, potentially life-threatening condition that occurs when there is too much serotonin activity between the synapses.
- Management varies on the severity of the condition.
- This condition does not occur in all individuals who take antidepressant medications.
- Keeping an eye out for these symptoms can help with managing the condition.
Read more: Natural ways to boost dopamine and serotonin levels