US researchers from Harvard Medical School have devised a modified technique to eliminate the inflammatory response seen in dopamine-producing stem-cell transplants for Parkinson’s disease. This study paves the way for advancing stem cell therapy, especially for drug-resistant Parkinson’s.
Dopamine is a key neurotransmitter that regulates body movements. In people with Parkinson’s, the brain loses neurons that produce dopamine.
Implanting dopamine-producing stem cells in the brain is a therapy that is gaining ground as a treatment option for Parkinson’s. However, the surgical procedure of seeding the cells causes local inflammation, kickstarting the immune system. As a result, the immune response destroys the dopamine-producing neurons, leading to a failed treatment.
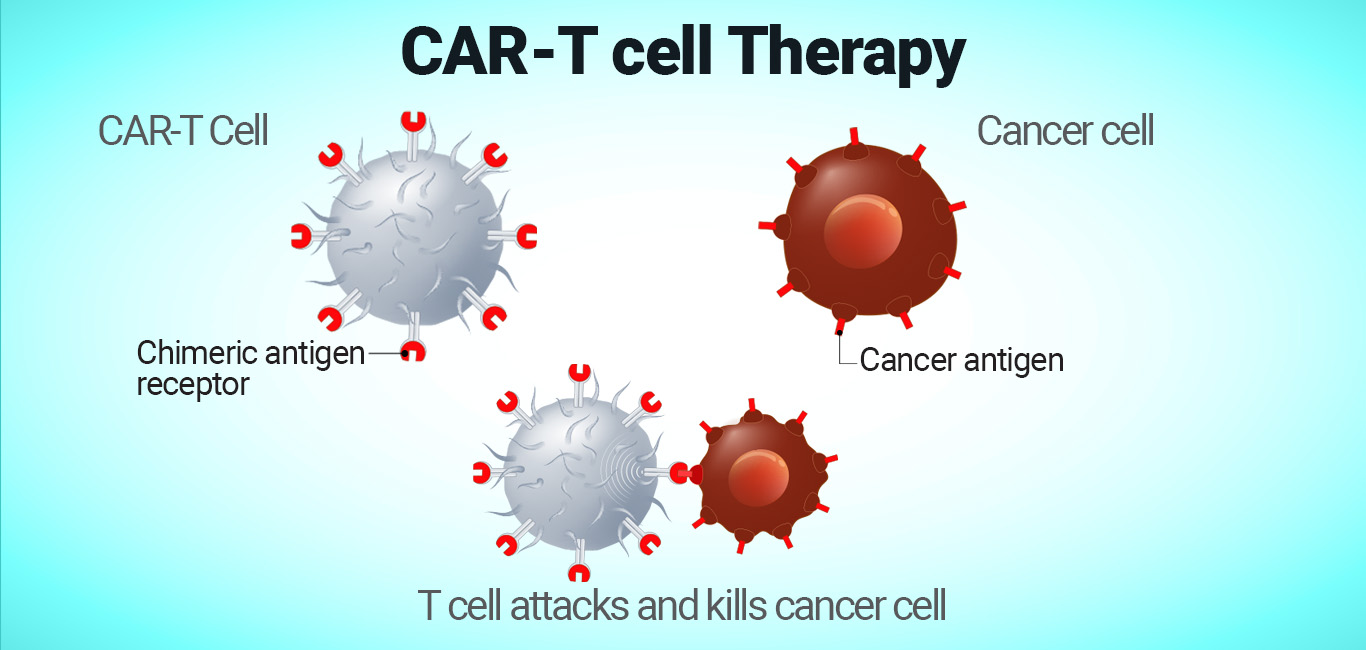
In this new technique, the researchers added immune cells called T-regulators to the stem cells that generate dopamine-producing neurons. When these modified cells were implanted in mice’s brains, they found no inflammation and the dopamine neurons survived.
A novel way to protect the stem-cell transplants
Dopamine is produced by the mid-brain dopamine neurons and is initiated by an enzyme called tyrosine hydroxylase. In their experiments on mice, the researchers observed that implanting neuronal stem cells with the enzyme helped produce dopamine, but the cells died soon due to inflammation. In other words, T-regulator cells around the implant site recognise the enzyme as an external particle. Therefore, inflammation develops around the surgery site.
Dr Kim says, “T regulatory cells play a major role in the immune response.” In comparison, those stem cells without the enzyme gave rise to surviving neurons.
“We demonstrated that this inflammatory response affects the survival of transplanted [dopamine-producing] neurons – tyrosine hydroxylase positive neurons. This, in turn, reduces the impact of the intervention on the clinical outcome,” says Dr Kwang-Soo Kim, Molecular Neurobiology Laboratory, Department of Psychiatry and McLean Hospital, Harvard Medical School, Belmont, USA.
So, to circumvent inflammation response in neighbouring cells, they added the immune T-regulatory cell as part of the stem cell with the enzyme. The stem cells were obtained from a human donor with Parkinson’s.
To test the efficacy of the modified cells, they replaced the mouse’s immune cells with those extracted from a person with Parkinson’s. They then took dopamine-generating stem cells from the same donor and added the enzyme to these cells. They observed that the immune system did not recognise the enzyme as a foreign particle; hence, there was no inflammation. The dopamine-producing neurons survived.
The current study’s novelty is that the team could experiment with human-derived stem cells in mice with human-like immune cells.
Dr Kim said that delivering the T-regulatory cells with transplanted cells masked the transplanted ones from eliciting an immune response against them, rendering the stem-cell therapy successful.