Animals such as dogs have an acute sense of smell, and pet parents vouch for their pets’ ability to sniff out changes in their health. Research has shown that some animals can even ‘smell’ cancers.
It turns out that even humans have similar abilities. A new study published in Nature found that our brain could ‘sniff out’ an infection as soon as it enters our nose.
Scientists tapped into the neural route that explains why we sometimes get a premonition of becoming ill even before the symptoms appear.
“This study helps us to understand a basic mechanism of detecting pathogens and how that’s related to the nervous system, which until now has been largely mysterious,” Dr Stephen Liberles, senior author of the study and a professor in the Blavatnik Institute at Harvard Medical School, said in a statement.
Dr Libreles and his team found a group of neurons in the nose that alerts the brain about the presence of pathogens. His team is the first to map this connection between respiratory infections and the brain.
Airway to brain
The team looked into how the influenza-A virus affected mice’s airways and brains. They observed that the infection decreased the mice’s appetite, water consumption, movement, and body weight, just as in humans.
They also noticed a spike in a molecule commonly produced in response to infections – PGE2 (prostaglandin E2). Various cells produce PGE2, which regulates the body’s response to infection by raising body temperature, increasing blood flow, altering blood pressure, and sensitising pain receptors.
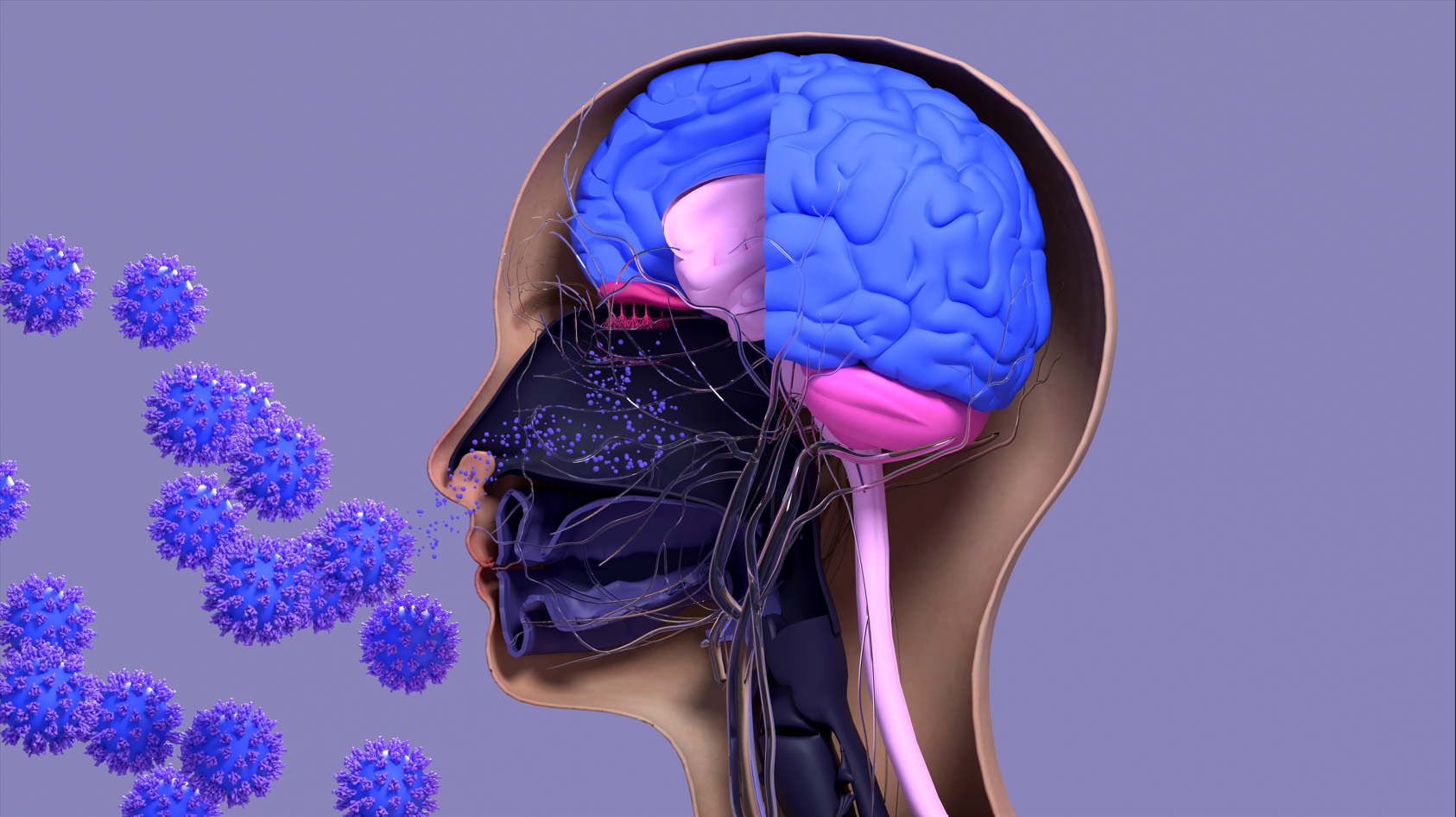
The earlier understanding was that PGE2 travelled through the bloodstream, crossing the blood-brain barrier and caused symptoms of sickness or sickly behaviour. However, Libreles’ team discovered that this sensation is perceived in the nose through a nose-nerve-brain connection.
Picture this: a vagrant respiratory virus floats into our nose and sits inside. Immediately, the immune system flags the uninvited guest’s presence by releasing PGE2 as the first line of response. This PGE2 in the nasal passage is detected by the glossopharyngeal nerve (GP). The GP connects to the hypothalamus in the brain that oversees the body’s responses like temperature, blood pressure, hunger and more. It sets off a series of events linking the brain to the immune response to infection, inducing a sense of feeling sick.
Read more: Hypothalamus: the brain’s smart coordinating centre.
Block to stop infection?
This is where the study gets interesting. The team used four individual strategies to see how this airway-neuron connect works. They ‘knocked out’ the genes that detect PGE2, suppressed the infection with ibuprofen (widely used painkiller), cut the GP nerve, and finally, neurons from the hypothalamus linking to the GP nerve.
All four strategies showed one common outcome: symptoms of sickness were diminished. As each method of validation was a form of PGE2 signal being interrupted, the team thinks that it has a role to play in reducing infection.
“Perhaps, the lack of prostaglandin signalling is promoting the immune system somehow to help reduce viral loads. And that increases survivability and better outcomes,” Dr Na Ryum Bin, first author of the study, told Happiest Health.
“And if we [carry out] genetic manipulations, apply ibuprofen, specific prostaglandin receptor antagonists [prostaglandin blockers], or even have the glossopharyngeal ablated (removed), we are able to eliminate the first phase of the sickness,” says Dr Ryum Bin.
The team has found that limiting the body’s response to a virus right from the start could prevent a full-blown infection.
The Indian scenario
Dr Narayan, ENT specialist and pulmonologist at Sri Satya Sai Hospital, Bengaluru, says that removing a nerve is not feasible at a clinical level. Instead, “[One] may have to do comparison study on flu patients with or without ibuprofen,” adds Dr Narayan.
While Dr Latha B C, consultant physician, Bengaluru, says that ibuprofen is not typically prescribed in India, making it difficult to substantiate this observation on a clinical level.
Delving deeper
In their future study, the research team intends to look closer at the neural response to the infection once it has reached the lower respiratory tract and lungs. Here, the infection is presumed to be independent of PGE2 secretion.
Dr Ryum Bin says that the most exciting part may come when they find the neurons that mediate the infection in the lungs. He theorises that isolating and manipulating the neurons, together with ibuprofen, will block the sickness condition altogether.
Future plans by the researchers include stopping the infection as soon as even the smallest symptom appears.