A common condition experienced by women, vaginitis is an inflammation of the vagina that brings about discharge, itching and pain. It is usually caused by an infection or an imbalance in the vaginal bacteria.
Take the case of Gunjan Malik (name changed), 38, a homemaker from Delhi, who started having an unusual discharge along with a lot of itching, post the birth of her second child. “At first, I thought it had something to do with my post-pregnancy issues as I was not in optimum health, and I also had an exceedingly difficult [vaginal] delivery. But after my gynaecologist did a physical examination, she told me it was vaginitis and prescribed some tablets. I had to complete two courses of antibiotics before I got some relief.”
READ MORE :
Can periods lead to a restless sleep pattern?
What menstrual blood colour reveals about health
What leads to vaginitis?
Dr Pooja Vyas Bansal, consultant gynaecologist, Cloud Nine Group of Hospitals, Navi Mumbai (Vashi), says, “There is usually a lot of unusual discharge, also itching because the normal flora – the bacteria – present there gets imbalanced. It can happen at any time or even during menopause when there is a drop in hormones. There are many types of vaginitis, but the most common types are bacterial and fungal. There are also some sexually transmitted ones like chlamydia, gonorrhea, trichomoniasis and HPV infection that can lead to pain and vaginal inflammation associated with vaginitis. It [vaginitis] could also happen because of infection or menopause or certain chemicals, soaps, sprays and vaginal washes”
Experts say vaginitis can occur in most women who are going through certain hormonal changes, such as those associated with pregnancy, birth control pills or menopause. Products such as bubble baths, vaginal spray or vaginal deodorants can cause it.
Douching (means showering the vaginal area with water), sexual activity, use of spermicides for birth control, sexually transmitted infections, diabetes, medications like antibiotics and steroids, using an intrauterine device (IUD) for birth control, wearing damp clothing can all bring it about.
Dr Bansal explains the most common types of vaginitis:
Bacterial vaginosis. This is the most common type of vaginitis. It results from a change in the bacteria found in the vagina, upsetting the balance. What causes the imbalance is unknown.
It is possible to have bacterial vaginosis without symptoms.
This type can be linked to but not caused by sex — especially if one has multiple sex partners or a new sex partner. But it can also occur in women who aren’t sexually active.
Yeast infections. This happens when there is an overgrowth of a fungal organism — usually candida albicans — in the vagina. This can also cause infections in other moist areas of the body, such as the mouth (thrush), skin folds and nail beds.
Trichomoniasis. This sexually transmitted infection is caused by a parasite called trichomonas vaginitis. It can spread during sex with an infected person.
Non-infectious vaginitis: It is an allergic reaction that can be caused by vaginal sprays, douches, perfumed soaps, scented detergents and spermicidal products that irritate the vulvar and vaginal tissues. Foreign objects like toilet paper or forgotten tampons in the vagina can also cause this. A form of non-infectious vaginitis – vaginal atrophy (atrophic vaginitis) – can thin, dry and inflame the vaginal walls when the body has less estrogen, during and after menopause.
Inflammation in vagina: What are the effects?
People with conditions like trichomoniasis or bacterial vaginosis can get sexually transmitted infections because of the inflammation caused by these disorders.
Experts suggest that one must connect with a doctor if there are symptoms like a strange, coloured discharge from the vagina, itching, irritation, pain during sex, painful urination, foul odour, light vaginal bleeding or spotting.
Treatment and prevention of vaginitis
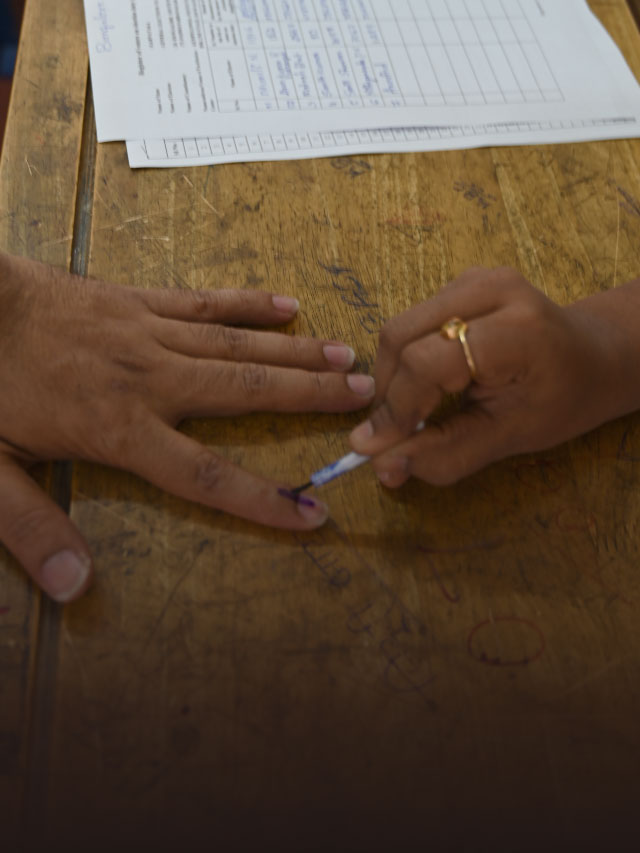
Treatment will depend on the type of vaginitis. Medical practitioners ask people to provide a sample of cervical or vaginal discharge for lab testing. A vaginal pH test may also be performed, which is a simple way to measure how acidic or alkaline the vaginal secretions are. Elevated pH levels may signal a vaginal infection.
“Treatment depends on the findings of the examination such as a Pap smear test or vaginal swabs. Usually, antibiotics are taken and local hormones can help,” says Dr Bansal.
According to Dr Karnika Tiwari, gynaecologist and obstetrician at Motherland Hospital, Noida, vaginitis is very common and it can happen to any woman. “That said, some women have a recurring issue, but it is nothing that can’t be treated,” says Dr Tiwari.
“In fact, we usually advise that women should practice good vaginal hygiene like wearing only underwear that is dried in the sun and not fan-dried. The former method means there are fewer bacteria in clothes,” adds Dr Tiwari.
Dr Bansal says that the preventive measures include avoiding physical intercourse without a condom and avoiding tight clothing or underwear and wet clothes. “Avoid douching and having sex with multiple partners and be regular with your pap smear,” advises Dr Bansal.
Dr Tiwari points out that one should also be careful whilst using public toilets as it can not only cause vaginitis but also lead to urinary tract infections. Frequent vaginitis can also be an indication of diabetes.